Sleep deeply and wake refreshed, as many of our patients already do after treatment at Liv Hospital!
Sleep
Expertise
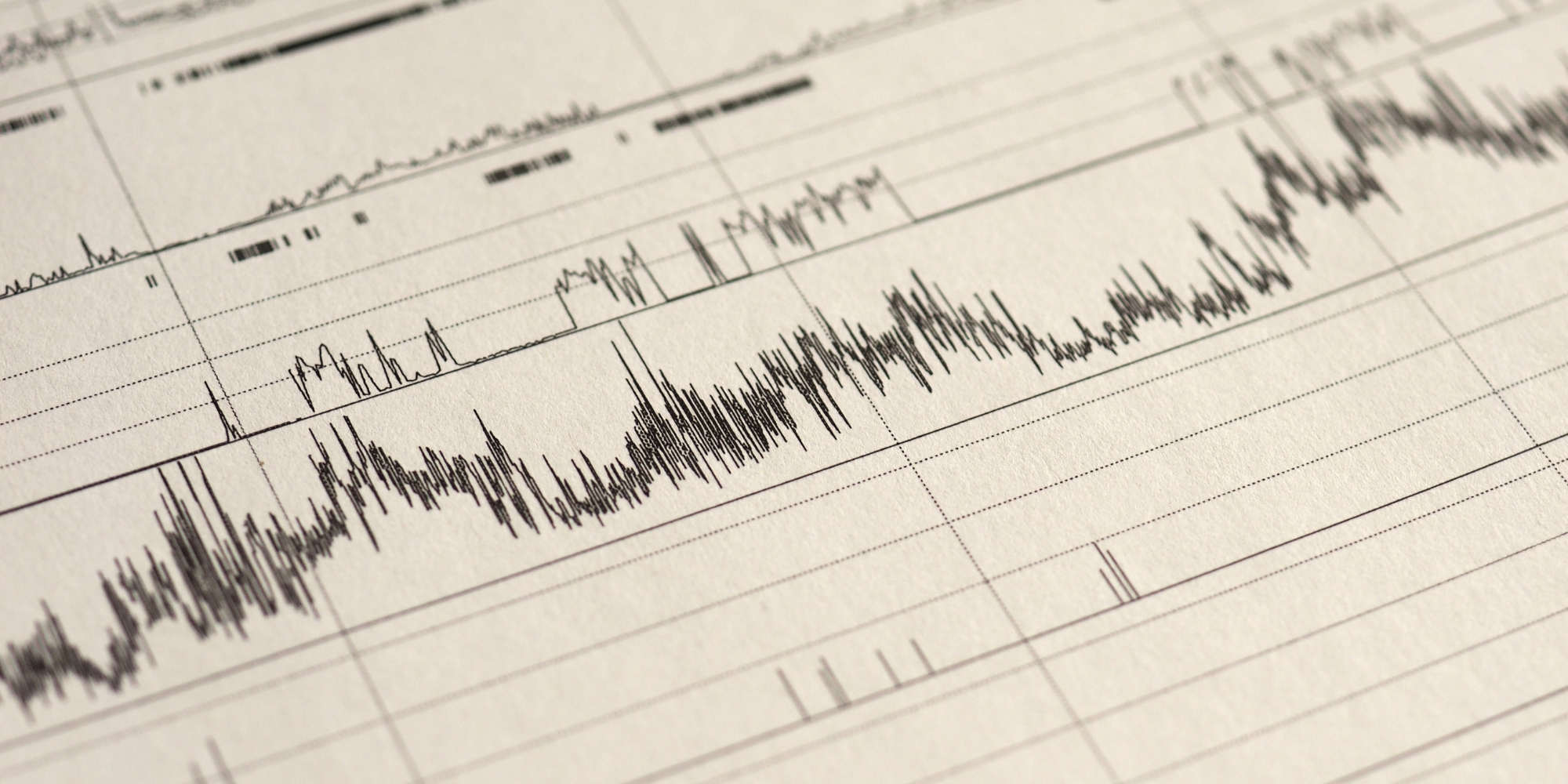
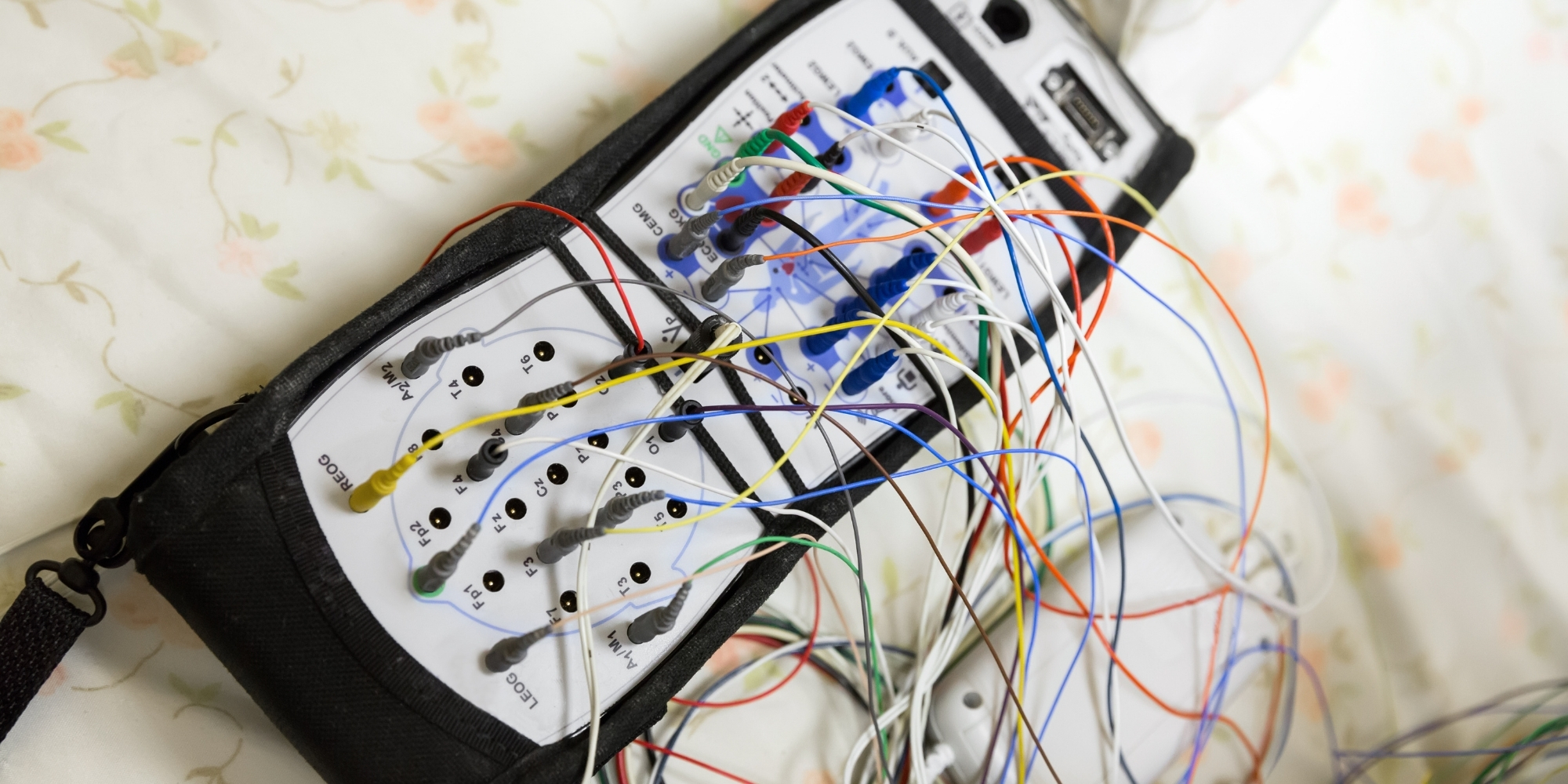
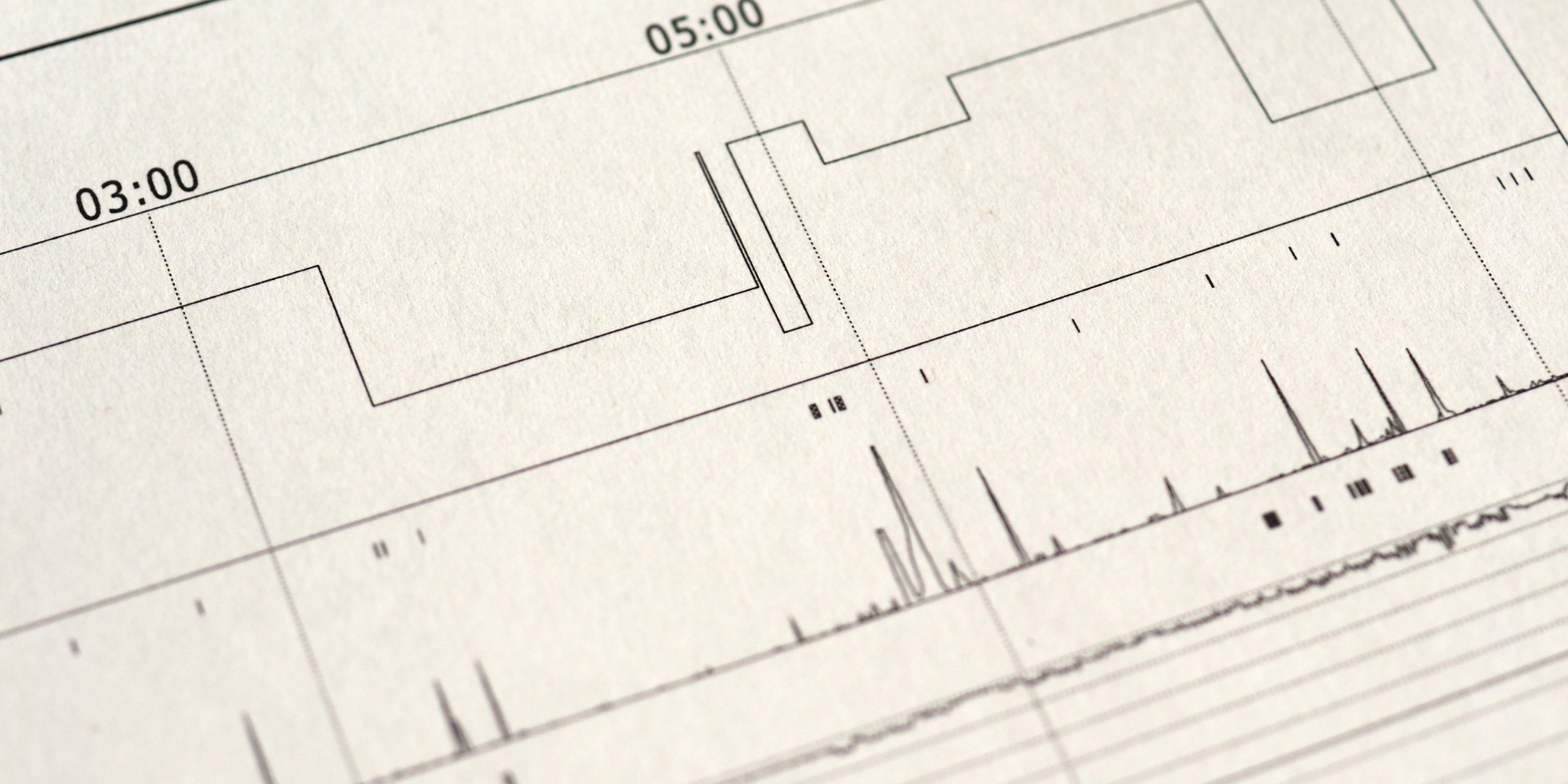
Experience advanced diagnostics and tailored care at Liv Hospital Dubai’s Sleep Study unit, specializing in sleep apnea solutions. Our specialists use cutting-edge methods to improve breathing, sleep quality, and overall health effectively and safely. This service reflects not only treatment, but the expertise, dedication, and precision supporting every patient’s journey.
Dr. Fabrizio Facchini
Consultant - PulmonologyWith over 15 years of international experience, this pulmonologist specializes in asthma, allergies, and sleep apnea. He is trained in advanced respiratory diagnostics, allergy testing, and comprehensive sleep studies. As a clinical leader, he has directed tertiary respiratory clinics and developed patient-focused care protocols. Skilled in bronchoscopy and multidisciplinary management, he combines precision medicine with compassionate care to improve breathing and sleep quality.
Curious about your respiratory health?
Explore Pulmonology advanced diagnostics, personalized care, and better breathing.